NUTRITION
*NOTE - The following information is not intended as a substitute for appropriate medical and nutritional advice. You should work together with your doctor and your registered nutritionist to discuss nutrition concerns*
The physiological changes that occur during pregnancy require extra nutrients, protein, and energy to meet the demands of an expanding blood supply, a developing fetus, the growth of maternal tissues, and preparation for lactation. Many people have the impression that, when pregnant, a women just has to eat a little more than usual to compensate for the growing life inside them. The addition of more food to the pregnant mother's diet is just one part of the issue. A pregnant mother also needs to eat the right foods to nurture growth and replenish their increasing nutrient, protein, and energy needs.
Current recommendations suggest that women should increase their daily energy intake by approximately 100 kcal in the first trimester and 300 kcal in the second and third trimesters (3). It should be noted that these are average numbers and that daily energy requirements depend on basal metabolic rate and activity patterns. These vary from individual to individual, therefore, women should maintain an active lifestyle and allow their appetites to guide their energy intake. In this case, appetite refers to a women's response to internal hunger cues.
The average weight gain during pregnancy is 26 to 32 pounds (5), but it is important that women do not get discouraged about this weight gain. She should think to herself: I've built a healthy body for myself and my baby!
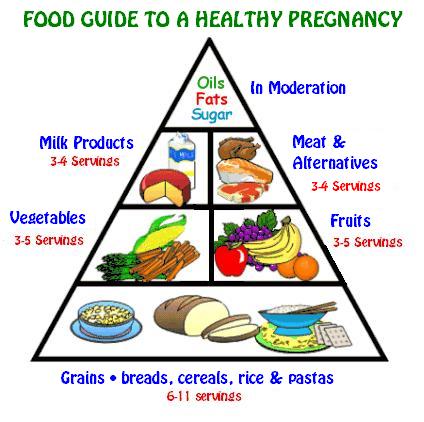
Table1. Recommended Daily Diet for Pre- and Postnatal Women
|
Food Group |
One Serving Is: |
Recommended Number of Servings For: | ||
| Pregnant | Postpartum & Breastfeeding | Postpartum & Not Breastfeeding | ||
| Milk Products |
250ml (1 cup) buttermilk 175ml (3/4 cup) yogurt 45g (1 1/2oz.) cheddar or processed cheese 125ml (1/2 cup) canned, evaporated milk, undiluted 75ml (1/3 cup) instant skim milk powder (dry) |
3-4 | 4-5 | 3-4 |
| Grain Products | 5g (1 slice) whole-wheat bread 125ml (1/2 cup) cooked cereal 175ml (3/4 cup) ready-to-eat cereal 125ml (1/2 cup) cooked rice (brown or
125ml (1/2 cup) cooked pasta, preferably whole grain 1/2 hamburger or hot dog bun 1/2 large roll or muffin 50ml (1/4 cup) pancake or waffle batter 1 15cm (6in.) diameter corn tortilla 1/2 English muffin, bagel, pita bread 4 graham wafers 6 soda biscuits |
6-11 | 6-11 | 6-11 |
| Fruits and Vegetables |
125ml (1/2 cup) vegetables/fruit - fresh or frozen 125ml (1/2 cup) juice- fresh frozen, or canned 1 medium sized potato, carrot, tomato, peach, apple, or orange 30ml (2 tbsp.) dried apricots, apples, or raisins 250ml (1cup) salad greens |
5-10 | 5-10 | 5-10 |
| Meat and Alternatives |
60 to 90g (2 to 3oz.) cooked lean meat, fish, poultry, or liver 60ml (4 tbsp.) peanut butter 250ml (1 cup) cooked dried peas, beans, or lentils 125ml (1/2 cup) nuts or seeds 60 to 90g (2 to 3 oz.) cheddar cheese 110 to 165g (1/2 to 3/4 cup) cottage cheese 2 eggs 150 to 21g (5 to 7oz.) tofu |
3-4 | 3-4 | 2-3 |
* Some foods other than those that fall into these food groups may be eaten as well. Many of these foods are higher in fat or calories, so it is best to consume these foods in moderation.
A lot of women find it difficult to consume adequate amounts of folic acid (folacine), calcium, vitamin D, and iron. For this reason, special attention needs to be paid to these nutrients during pregnancy.
Table 2. Important Vitamins and Minerals for Pregnant Women
| Vitamin/Mineral | Importance |
Sources |
Special Notes |
| Folic Acid | - supports pregnant women's expanding blood
volume and growth of maternal and fetal tissues
- decreases the risk to the fetus of neural tube defects |
- dark green, leafy vegetables - citrus fruits and juices - peanuts - wheat germ - whole grain and enriched grain products |
- women should consume 400ug/day (4)
- it is especially important for women to increase their folic acid intake before becoming pregnant and continuing through the first 3 months to reduce the risk of babies having a neural tube defects (3) |
| Calcium | - hardens and strengthens bones and teeth
- provides for skeletal development of the fetus - aids in production of breast milk |
- milk - cheese - yogurt - tofu set with calcium sulphate |
- if a woman does not drink milk, or eat,
yogurt, or cheese daily, they should talk to a doctor about taking a
calcium supplement
- recommended nutrient intake for pregnant women is 1200 - 1500mg/day (3) |
| Vitamin D | - helps body absorb calcium
- essential for body to use calcium efficiently |
- cow's milk - fortified soy beverages - fatty fish (e.g. salmon) |
- recommended nutrient intake for pregnant women is 5ug or 200IU/day (3) |
| Iron | - needed to increase the maternal blood cell
mass and to supple the growing fetus and placenta
- baby needs iron until his or her diet includes iron rich foods (at about four to six months of age) (6) |
- clams, oysters - red meat - dried beans - whole grain and enriched cereals - tofu -dark green, leafy vegetables |
- vitamin C enhances iron absorption
- recommended nutrient intake for pregnant women increases from 13mg to 18mg in the second trimester and to 23mg in the 3rd (3) |
 Postpartum Nutritional Tidbits
Postpartum Nutritional Tidbits
If a new mother is going to breastfeed the recommended daily allowance (RDA) calls for an increase in caloric intake of 500 calories above one's normal energy requirements (7). A recommended daily diet for a breastfeeding mother can be seen in table 1 above. Moderate to caloric restriction is not advised during breastfeeding because it may diminish the quality of the milk. For women who are not breastfeeding their baby, they may return to their normal caloric intakes.
Most women experience only a 10- to 14-pound weight loss at delivery. An additional 4 to 7 pounds is lost in the first week as excess body fluid is eliminated and the uterus approaches its normal size (7). Most women want to return to their ideal weights sooner than later after pregnancy. Postpartum weight loss may be enhanced by engaging in an exercise program and making wise nutrition choices. These chose are very simple and could be applied to a women who has not just given birth. In order to assure gradual weight loss it is important to avoid the extra calories found in candies, chips, pops, etc. The new mother should try to avoid fried foods, drink low-fat or non-fat milk, and eat chicken and fish instead of beef and pork.
Very active mothers, such as mothers participating in a rigorous exercise program, who are still breastfeeding may find that they have to consume many calories in order to maintain their ideal weight.
Exercise, Pregnancy and Nutrition
When a woman is pregnant and participating in an exercise program it is essential that she makes sure she is eating enough calories to support her pregnancy and the physical activity she is performing. This becomes a problem as many fit women tend to reduce their caloric intake during pregnancy. An inadequate intake of calories will cause the body to use protein as an energy source instead of for tissue building, thus fetal growth may be affected. In most cases, caloric intake should not drop below 36 kcal per kilogram or 16 kcal per pound (7).
Pregnant women who are participating in a physical activity should bring a snack along with them in case they start to feel hungry, light-headed, or shaky, which are all signs of hypoglycemia (abnormal decrease of sugar in the blood). Pregnant women who exercise should always carry a water bottle of some sort with them at all times as the risk of dehydration is increased during pregnancy. Dehydration can raise the woman's core body temperature to dangerous levels.
** The best way to make sure caloric needs are being met are to pay attention to your appetite and weight gain **
Safeguards for Eating and Foods to Avoid
Once a woman is trying to conceive it is recommended that she stop consuming certain foods that may be harmful to the fetus. Many of these harmful foods have their biggest influence during the first trimester, therefore, the earlier they are eliminated from the diet the better.
Caffeine
The evidence about the effects of caffeine on babies is mixed, but several studies have shown evidence of birth defects (5).Other studies have found that the consumption of caffeine in moderation is not believed to have any adverse effects on pregnancy or on the fetus. Limiting caffeine intake while lactating is important because caffeine appears in breast milk (3). Pregnant and lactating women should limit the amount of caffeine they consume to no more than 400-450mg (less than 3.5 cups of strong tea) of caffeine a day (3).
Sweeteners
Evidence suggests that consumption of artificial sweeteners by pregnant women is safe and does not pose a health hazard (3). Pregnant women should not consume excessive amounts of artificial sweeteners which are low in nutrient value, for example, diet soft drinks, because such foods could be replacing nutrient-rich foods.
Contaminants
Contaminants can exist naturally in many foods or can come from pollution. This is a great concern for pregnant mothers as even a little bit of contamination can affect the health of the baby.
To protect against lead contamination, fruit juices and acidic foods should be stored in glass or plastic containers rather than leaded crystal or ceramic containers - in older homes with lead pipes and faucets, water should be filtered (5)
Large fish can be contaminated with mercury and fresh fish can also be contaminated with pesticides and polychlorinated biphenyls (PCBs) - because these toxins usually accumulate in fat, stick with low-fat fish and where possible, trim the fat off of the fish you eat (5)
To protect against food-borne parasites (3):
avoid consumption of raw meats, including fish and poultry, raw eggs and unpasteurized dairy products.
avoid cross-contamination between raw foods and cooked foods.
do not store fresh or cooked meat and poultry products for more than 2-3 days in the refrigerator
wash all raw fruits and vegetables thoroughly
make sure hot foods are hot (above 60oC/140oF), cold foods are cold (below 4oC/39oF), and that all meats are well cooked.
soft cheeses and pÔtÚs may be sources of Listeria monocytogenes and should be avoided during pregnancy.
wash hands prior to food preparation, and wash and disinfect (with household bleach) food preparation surfaces and utensils that have been in contact with raw food.
Water
It is important to drink 6-8 glasses of water a day when pregnant. Water serves many important functions in the body and one of these is transportation of nutrients throughout the body. It also works in conjunction with fibre to prevent constipation (6). As food intake increases with pregnancy, the need for water also increases. As mentioned above, it is extremely important to drink more than 6-8 glasses of water a day if you are a pregnant women participating in an exercise program and it is a good idea to have a water bottle with you at all times.
Pregnancy and Vegetarianism
In most cases, well-planned vegetarian diets support good nutritional status and health. However, ensuring nutritional adequacy becomes more challenging as more types of food are avoided and when nutrients needs are higher, such as during pregnancy.
Iron deficiency becomes an issue for many pregnant women who practice an vegetarian diet. If a pregnant women has a well chosen vegetarian diet she will have no problem obtaining and adequate amount of iron. These diets generally include high intakes of vitamin C which promotes increased absorption of iron. Pregnant women following a vegetarian diet may also be in danger of acquiring enough vitamin D in their diet. Vegans are especially at a high risk of vitamin D shortage as well as vitamin B12 which is only available from animal sources. Vegans should consume at least 1 ug of vitamin B12 a day by taking a supplement or eating fortified foods such as meat analogues (3). The bottom line for vegan women who are pregnant or who are planning a pregnancy should consult their doctor and a registered nutritionist for a dietary assessment and counseling.
Points of Interest
Gestational diabetes (GD) occurs when pregnancy alters the way a woman's body takes up sugar. In normal cases, insulin helps move blood sugar (glucose) into muscles and organs. When suffering from gestational diabetes, insulin levels are too low, so the amount of glucose in the blood rises to dangerous levels while muscles and organs don't get enough (4).
Gestational diabetes is the most common complication of pregnancy, affecting 3-6% of pregnant American women (2). Exercise has a role in treatment and , perhaps, even prevention of GD. Traditional treatment also involves a diet that limits carbohydrate intake (4). Exercise can play a major role in controlling blood glucose levels in women who develop GD. Exercise can do this without insulin because contracting muscles help stimulate glucose transport. A contracting skeletal muscle can increase its glucose uptake 35-fold (1).
The American Diabetes Association endorsed exercise as "a helpful adjunctive therapy" for GD when high levels of glucose are not affected by diet alone (2). One study conducted, used a fairly high-intensity exercise regimen and resulted in normoglycemia (normal blood glucose levels) within 1 week. The protocol that was used in this study is currently implemented in many clinical settings (2).
Pregnant women who suffer from GD must be cautious and take particular precautions when exercising. These precautions include, monitoring blood glucose, regulating meal times, scheduling periods of rest, and carefully tracking fetal activity and uterine contractions.
Exercise programs undertaken by pregnant women who have GD should be individualized and conducted under careful medical supervision.
NOTE - The above information is not intended as a substitute for appropriate medical and nutritional advice. You should work together with your doctor and your registered nutritionist to discuss nutrition concerns.
References
1. Artal, R. (1996). Exercise: An alternative Therapy for Gestational Diabetes. The Physician and Sportsmedicine, 24 (3).
2. Artal, R. & Sherman, C. (1999). Exercise During Pregnancy. The Physician and Sportsmedicine, 27 (8).
3. Health Canada. (1999). Nutrition for a Healthy Pregnancy: National Guidelines for the Childbearing Years. Ottawa: Minister of Public Works and Government Services Canada.
4. Healthtrack. (1996, July). Your Pregnancy : Expect the benefits of Exercise. A Supplement to The Physician and Sportsmedicine For The Waiting Room.
5. Kleiner, S.M. (1996). What to Do When You're Eating for Two. The Physician and Sportsmedicine, 24 (3).
6. Ministry of Health, Province of British Columbia. (1992). Baby's Best Chance (3rd ed.) Toronto: Macmillan.
7. Vega, C. (1987, March). Maternal Nutrition. Dance Exercise Today, p 65-68.
(Exercise on your Body) (Effects of Pregnancy) (Exercise Guidelines)
(Precautions & Contraindication) (Benefits of Exercise) (Exercise Programs) (Perinatal Dangers)
(Hints for Around the House) (Tips for Fitness Instructors)